For over a decade, Kaiser Permanente has faced scrutiny over its mental health care services, despite its strong reputation in the medical field. In 2013, the insurer was fined $4 million by California regulators for failing to meet standards in reducing wait times, providing accurate information to patients, and managing appointment data. Fast forward to 2023, and KP agreed to a $50 million settlement, the largest fine ever imposed by the state’s Department of Managed Health Care, for similar violations.
Currently, Kaiser Permanente is embroiled in a contentious situation as mental health workers in Southern California are in the fourth month of a strike. Therapists and union representatives claim that the healthcare giant overloads workers with excessive caseloads, leading to long wait times for patients seeking follow-up appointments. They argue that the staff is burnt out, making it challenging to recruit new clinicians and worsening the staffing crisis.
On the other hand, Kaiser Permanente denies these allegations, dismissing them as outdated issues brought up by the union to tarnish the organization’s reputation. They maintain that their commitment to delivering quality, affordable care contradicts the union’s demands for higher pay. With approximately 9 million members, Kaiser Permanente is the largest commercial health plan in California, facing challenges in providing adequate mental health care, exacerbated by a nationwide shortage of healthcare workers.
##
Challenges in Mental Health Care
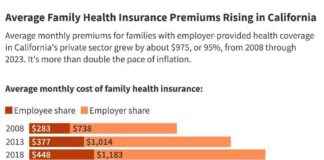
Federal and state laws mandate health plans to offer mental health care that is on par with medical care, known as mental health parity laws. However, the implementation of these laws has been inconsistent, with many patients struggling to find therapists within their insurance networks. Surveys reveal that a significant number of listed providers do not respond to inquiries, a trend that is more prevalent in mental health and substance abuse care compared to medical services.
Furthermore, California regulators have initiated behavioral health care investigations into various health plans to address delays in care. While the Department of Managed Health Care has identified numerous violations and barriers affecting patient access to mental health services, the challenge remains in reconciling the open-ended nature of therapy with the financial constraints faced by health plans.
Mark Peterson, a professor at UCLA’s Luskin School of Public Affairs, highlights the conflict between therapy duration and cost management for insurers. The reluctance of therapists to accept insurers’ payment rates often leads to their exclusion from health plan networks, making therapy financially inaccessible to many individuals.
##
Struggles at Kaiser Permanente
Within California, Kaiser Permanente accounts for a significant portion of mental health-related fines imposed by the DMHC. Despite facing penalties and criticisms, Kaiser Permanente asserts that it has invested over $1 billion in expanding treatment facilities and hiring more mental health providers since 2020. The ongoing strike by mental health workers in Southern California underscores the challenges faced by frontline staff, demanding higher wages, reduced patient loads, and improved working conditions.
Kassaundra Gutierrez-Thompson, a Kaiser Permanente therapist involved in the strike, sheds light on the harsh realities of working conditions within the organization. Citing instances of colleagues suffering from urinary tract infections due to excessive workloads, Gutierrez-Thompson emphasizes the dehumanizing factory-like environment that impedes quality patient care. Her personal experience as both a provider and patient within the Kaiser Permanente system adds a poignant layer to the ongoing debate, illustrating the urgent need for reforms in mental health care services.
As the healthcare landscape grapples with systemic challenges in delivering mental health care, the plight of Kaiser Permanente serves as a microcosm of broader issues affecting the industry. While the organization strives to address deficiencies and enhance patient access to mental health services, the voices of frontline workers like Gutierrez-Thompson highlight the critical need for sustainable solutions that prioritize both quality care and staff well-being.
This insightful article, produced by KFF Health News, showcases the complexities of mental health care delivery within a prominent healthcare provider, urging stakeholders to reevaluate existing practices and work towards a more compassionate and effective system that prioritizes patient outcomes and staff welfare.