The Trump administration recently unveiled a series of proposed changes to the Affordable Care Act, raising questions about whether these alterations are intended to enhance consumer protection or complicate the enrollment process. The policy experts have weighed in, expressing concerns that these new regulations might make it more challenging for individuals to secure coverage, potentially leading to decreased enrollment rates.
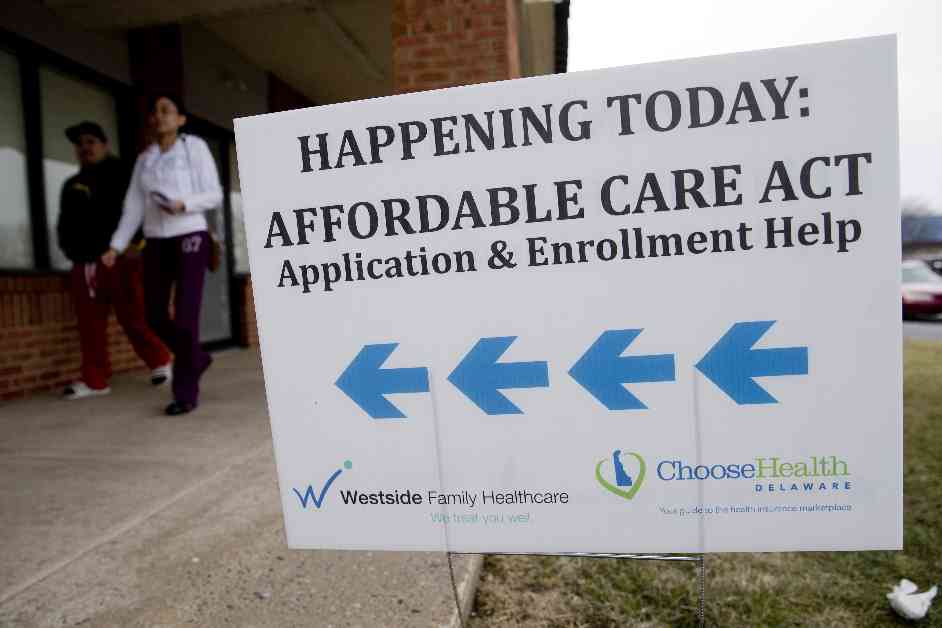
On Monday, the federal officials disclosed the details of the proposed changes, which were inadvertently released after a draft press release was published earlier. With around 24 million Americans signing up for ACA insurance plans in 2025, the Biden administration witnessed record enrollment figures after boosting premium subsidies for lower-income individuals. This initiative not only reduced the monthly costs of certain plans to $0 but also facilitated year-round enrollment for very low-income individuals, eliminating the need to wait for the traditional fall enrollment period. Unfortunately, the program faced an influx of fraudulent enrollments, prompting approximately 274,000 consumer complaints by August, primarily attributed to rogue insurance agents and other unscrupulous parties.
The Trump administration justified its new regulations as essential steps to safeguard consumers from unwittingly being enrolled in Marketplace coverage, promote stability in health insurance markets, and ensure that taxpayer funds support only those individuals intended to benefit from the ACA. However, policy experts like Sabrina Corlette, a research professor at Georgetown University’s Center on Health Insurance Reforms, worry that these changes might impose additional paperwork requirements that could impede enrollment efforts, particularly for low-income consumers.
Increased Documentation Requirements
The proposed changes introduce a series of new requirements for consumers, necessitating more detailed information to validate their eligibility for special enrollment periods and premium subsidies during the enrollment process. This includes shortening the annual enrollment period by a month and limiting eligibility for “Dreamers,” immigrants brought to the country illegally as children, based on the DREAM Act proposals. Furthermore, the proposal eliminates the year-round special enrollment period for individuals with very low incomes but establishes stricter verification protocols for other special enrollment scenarios, such as income changes or loss of job-based coverage.
Moreover, individuals auto-renewed into zero-premium plans during regular enrollment will be required to pay a nominal monthly fee until they update or confirm their information. The proposal also mandates additional data collection from consumers, particularly self-employed or gig workers, who estimate their income for the forthcoming year without prior tax return filings with the IRS.
Impact on Enrollment and Program Integrity
While some of the Trump administration’s changes aim to address unauthorized enrollments, such as notifying consumers of inadvertent ACA plan sign-ups, the increased paperwork and stringent eligibility criteria might deter certain individuals from enrolling. Cynthia Cox, a director at KFF, expressed concerns that these alterations could affect legitimate enrollees struggling to document anticipated income changes, potentially leading to enrollment declines.
Additionally, the proposal introduces changes to the ACA marketplaces, including ending the policy that allowed Dreamers to qualify for subsidized ACA coverage. Moreover, gender-affirming care would no longer be considered an essential health benefit, potentially resulting in higher out-of-pocket costs for individuals seeking sex-trait modification services.
As the proposed rule undergoes a public comment period, Katie Keith, a director at Georgetown University, highlighted that the full implementation of these changes may vary between 2025 and 2026. While acknowledging potential administrative challenges for consumers, the FAQ accompanying the proposal emphasized the importance of enhancing program integrity and deterring improper enrollments, despite possible adverse impacts on coverage accessibility.
In conclusion, the proposed changes to the ACA reflect a delicate balance between protecting consumers from fraudulent enrollments and minimizing barriers to enrollment. The ensuing public dialogue and regulatory revisions will shed light on the true implications of these alterations on the healthcare landscape.