Last Tuesday was a rollercoaster of emotions for state Medicaid staff nationwide, as a memo from the Trump administration initially threatened to freeze all federal financial assistance, including Medicaid funds. This sudden announcement left Medicaid agencies in a state of panic, temporarily locking them out of their U.S. Treasury accounts. However, just as quickly as the chaos ensued, the Trump administration backtracked, clarifying that Medicaid was exempt from the funding freeze. This episode shed light on the vulnerable position of Medicaid programs, often a target for political scrutiny, especially from Republicans.
The Uncertain Future of Medicaid
The original memo, which explicitly exempted Medicare and Social Security from the funding freeze but not Medicaid, raised eyebrows and highlighted the ongoing challenges faced by Medicaid programs. With the Trump administration’s aggressive push to extend tax cuts for the wealthy, Medicaid remains a prime target for budget cuts and reforms. The confusion surrounding the initial freeze forced the administration to provide clarification, but the underlying tension between political agendas and essential healthcare programs like Medicaid continues to simmer.
In the midst of this uncertainty, stories from current and former employees within state Medicaid agencies or the Centers for Medicare and Medicaid Services offer valuable insights into the real-world impact of such policy decisions. Their experiences shed light on the challenges faced by these vital healthcare programs and the individuals they serve, providing a human perspective on the complexities of the Medicaid landscape.
UnitedHealthcare’s Potential Coverage of Vertex’s Pain Drug
On a different front, Vertex Pharmaceuticals’ recent FDA approval of a new non-opioid pain drug, Journavx, has sparked interest in potential coverage by UnitedHealthcare, the nation’s largest health insurer. The need for non-addictive alternatives to opioid painkillers is a pressing issue, and the approval of Journavx presents a potential solution. However, questions linger regarding the drug’s effectiveness compared to existing pain management options.
Late-stage trials indicated that Journavx provided safe and modest pain relief, but its performance did not surpass a combination of acetaminophen and hydrocodone. UnitedHealthcare’s decision to potentially place Journavx on a non-preferred tier in their list of approved drugs, with a 20% coinsurance for most insured individuals, reflects the balancing act insurers face in providing access to innovative treatments while managing costs. The pricing of Journavx at $31 per day further underscores the financial considerations at play in healthcare decision-making.
The Evolving Landscape of Drug Sales and Coverage
The shifting dynamics of drug sales and coverage also come into focus with the case of Humira, a blockbuster rheumatoid arthritis treatment manufactured by AbbVie. After facing competition from cheaper biosimilar versions in 2023, U.S. sales of Humira declined but still amounted to a substantial $12.2 billion. The reluctance of pharmacy benefit managers to drop Humira, driven by concerns over rebates and client relationships, delayed the inevitable decline in sales.
In 2024, the tide began to turn as PBMs started to phase out Humira in favor of alternative options, leading to a significant drop in U.S. sales to $7.1 billion. Despite this decline, Humira’s sales figures underscore its enduring impact on the pharmaceutical market, positioning it as a formidable player in the industry. The evolving landscape of drug sales and coverage reflects the complex interplay between market forces, regulatory decisions, and patient needs.
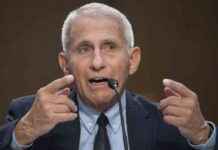
Navigating the Healthcare System: Annual Wellness Visits and Regulatory Oversight
As patients navigate the intricacies of the healthcare system, annual wellness visits emerge as a focal point for Medicare Advantage plans like those owned by UnitedHealth. These check-ins serve as a mechanism for collecting health data and generating billing codes, essential for the financial sustainability of these plans. The promotion of annual wellness visits by healthcare providers, while not always transparent in its motivations, reflects the broader strategies employed within the healthcare industry to optimize revenue streams.
Expert voices like Daniel Zingale, the former “HMO czar” of California, emphasize the need for regulatory oversight that prioritizes patient well-being over corporate profits. Zingale’s advocacy for a comprehensive regulatory overhaul underscores the longstanding challenges within the healthcare system and the imperative to address systemic issues that impact patient care. By amplifying stories like that of Margaret Utterbach, whose tragic experience with delayed treatment underscores the human cost of bureaucratic inefficiencies, Zingale calls for a more compassionate and patient-centered approach to healthcare regulation.
In a landscape shaped by industry trends, policy developments, and patient experiences, the complexities of the healthcare system come into sharp focus. From the potential coverage of innovative drugs to the regulatory challenges faced by healthcare oversight bodies, the narratives woven through these stories offer a multifaceted view of an ever-evolving industry. As stakeholders navigate the uncertainties and opportunities within healthcare, the need for informed dialogue, ethical decision-making, and patient-centered care remains paramount.